Solutions

MDsyncNET’s cloud-based software reduces inefficiencies, delivers immediate results, and maximizes ROI.
WHO WE SERVE

MDsyncNET delivers right-sized software to healthcare organizations in a variety of environments.
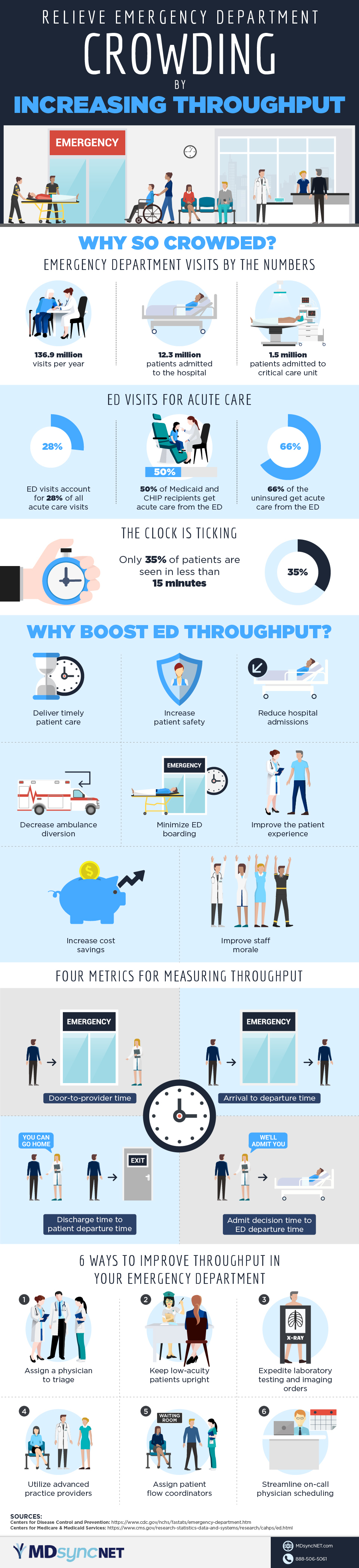
A hospital’s emergency department is on the front line of acute care, and emergency department crowding is itself an emergency. According to the Centers for Disease Control and Prevention, there are close to 137 million emergency department visits per year in the U.S. Of those patients, more than 12 million are admitted to hospitals and another 1.5 million are admitted to critical care units.
In 2016, an astounding one in five adults and 17 percent of children made one or more trips to the emergency department. In fact, the Centers for Medicare & Medicaid Services (CMS) reports that emergency department visits account for 28 percent of all acute care visits. Fully half of Medicaid and Children’s Health Insurance Program recipients and 60 percent of the uninsured obtain acute care from the emergency department. And, because of the Emergency Medical Treatment and Active Labor Act of 1986 (EMTALA), any person entering an emergency department must be provided with an exam and stabilizing treatment regardless of their ability to pay.
Overutilization of emergency departments results in crowding, and crowding means that sick patients have to cool their heels while waiting to be seen. In fact, the CDC notes that only about 35 percent of patients are seen in under 15 minutes. Delays in treatment have a number of implications, such as increased complication rates, increased hospital admissions, and increased boarding of patients in the emergency department. Other impacts can include the diversion of ambulances to other hospitals, higher costs in delivering care, lower staff morale, and decreased patient satisfaction.
Hospitals have many incentives to improve throughput in their emergency departments, but patient satisfaction is on track to become a driving motivator. CMS is piloting the Emergency Department Patient Experience of Care (EDPEC) survey, which is essentially HCAHPS for emergency departments. Early results indicate a direct correlation between a patient being seen within 30 minutes of arrival and how they rate their care.
Versions of EDPEC will likely target both patients admitted to the hospital – as an HCAHPS add-on – and patients who are discharged from the emergency department. Conceivably, like HCAHPS, this survey could be used in future CMS pay-for-performance initiatives.
Throughput can be measured using four criteria. The first is the time that elapses between a patient’s arrival in the emergency department and they time they are seen by a healthcare provider. The second is the length of time a patient spends in the emergency department, or the arrival-to-departure time. The third is the length of time between a patient being discharged and that patient actually leaving the emergency department. The fourth is the amount of time that elapses between the moment the decision is made to admit a patient to the hospital and the moment the patient actually leaves the emergency department.
Hospitals can implement a number of strategies to boost emergency department throughput. Here are the top six:
1. Assign a physician to triage. Decision-making is streamlined when there is a physician embedded in the triage process. That creates efficiencies that lead to a reduction in door-to-treatment time and patient arrival to departure time.
2. Keep low-acuity patients upright. Bedding a patient requires physical space and staff resources. Many low acuity patients can be screened while sitting in a chair in an evaluation area next to the waiting room.
3. Expedite laboratory testing and imaging orders. Ordering laboratory tests and imaging while a patient is in the waiting room or a nearby evaluation area removes the immediate need for a bed or gurney and lessens the patient wait time, thus improving the patient experience.
4. Utilize advanced practice providers. Nurse practitioners and physician assistants can evaluate and treat low-acuity patients. Depending on hospital policy, these advanced practice providers can be directly or indirectly supervised by emergency department physicians.
5. Assign patient flow coordinators. A nurse who is trained as a patient flow coordinator serves two purposes. First, they can communicate with patients in the waiting room about anticipated wait times, thus setting expectations that can serve to decrease the number of patients who leave without being seen and to increase patient satisfaction. Second, they can identify patients who are deteriorating and whose treatment should be prioritized.
6. Streamline on-call scheduling. Manual on-call scheduling processes lead to schedules that quickly become obsolete. This results in decreased throughput when the wrong on-call physician is contacted. In contrast, automated on-call scheduling helps ensure that the right doctor is called at the right time, so that patients can be seen quickly and either discharged or admitted.
Improving throughput is essential to reducing emergency department crowding. These and other strategies can help hospitals deliver value-based care that leads to higher staff morale and a better patient experience.
Download MDsyncNET's infographic, "Reliever Emergency Department Crowding by Increasing Throughput" here: https://mdsyncnet.com/wp-content/uploads/2019/01/mdsyncnet_crowding.pdf

© 2022 All Rights Reserved. MDSYNCNET | Privacy Policy & Terms and Conditions